Why and when do Obstetric Ultrasound
Wednesday,March 14,2018
Introduction to Obstetric Ultrasound
Obstetric Ultrasound is the ultrasound scans used in pregnancy. Since its introduction in the late 1950’s, ultrasonography has become a very useful diagnostic tool in Obstetrics.
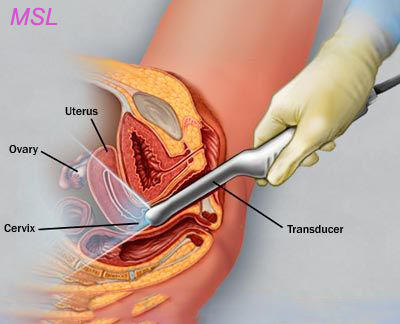
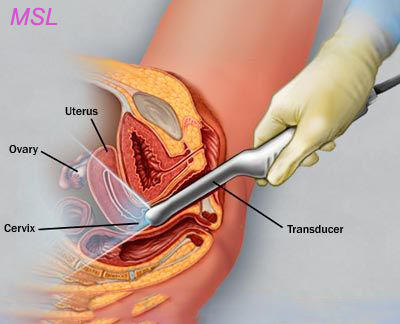
Currently used equipments are known as real-time scanners. It can capture a continous picture of the moving fetus and be depicted on a monitor screen. Very high frequency sound waves of between 3.5 to 7.0 megahertz (i.e. 3.5 to 7 million cycles per second) are generally used for this purpose.
They are emitted from a transducer which is placed in contact with the maternal abdomen, and is moved to "look at" (likened to a light shined from a torch) any particular content of the uterus. Repetitive arrays of ultrasound beams scan the fetus in thin slices and are reflected back onto the same transducer.
The information obtained from different reflections are recomposed back into a picture on the monitor screen (a sonogram, or ultrasonogram). Movements such as fetal heart beat and malformations in the feus can be assessed and measurements can be made accurately on the images displayed on the screen. Such measurements form the cornerstone are in the assessment of gestational age, size and growth in the fetus.
A full bladder is often required for the procedure when abdominal scanning is done in early pregnency. There may be some discomfort from pressure on the full bladder. The conducting gel is non-staining but may feel slightly cold and wet. There is no sensation at all from the ultrasound waves.
Why and when do Obstetric Ultrasound?
Ultrasound scanning is currently considered as a safe, non-invasive, accurate and cost-effective study of the fetus. It has gradually become an indispensable obstetric tool and plays an important role in the care of every pregnant woman.
The main uses of ultrasound are the following aspects:
1. Early pregnancy diagnosis and confirmation.
Pregnancy sac can be four and a half weeks of pregnancy and about five weeks of pregnancy can be seen at the yolk sac. Embryos can be observed and measured for about five and a half weeks. Ultrasound can also be very important to confirm the pregnancy site in the uterine cavity.
2. Early pregnancy vaginal bleeding.
Vaginal bleeding in early pregnancy can be recorded when the survival rate of the fetus. Visible beats can be seen and detected by pulsed Doppler ultrasound for approximately 6 weeks, and can usually be clearly depicted within 7 weeks. If you find this situation, the probability of continuing to be pregnant is better than 95%. Missing aborted and damaged eggs usually give typical pictures of a deformed gestational sac with no fetal bars or heart beats.
Fetal heart rate in early pregnancy changes with gestational age. The normal heart rate at 6 weeks is about 90-110 beats / min (bpm) and 140-170 beats / min at 9 weeks. At 5-8 weeks, bradycardia (less than 90 beats / min) is associated with a high risk of miscarriage.
Many women do not ovulate on day 14, so the results of one scan should be interpreted cautiously. Misdiagnosis of miscarriage is usually diagnosed by continuous ultrasound scan to prove the lack of pregnancy. For example, if an ultrasound scan shows a 7mm embryo but does not show a clear heartbeat, missed miscarriage can be diagnosed. In this case it is reasonable to repeat the ultrasound scan within 7-10 days to avoid any errors.
In this regard, the timing of pregnancy-positive tests may also help to assess the possible date of conception. For example, a positive pregnancy test conducted 3 weeks ago showed a gestational age of at least 7 weeks. This information is useful for the interpretation of the scan. Please read the FAQ for more comments.
Ultrasonography is also essential for the early diagnosis of ectopic pregnancy and molar pregnancy in cases of early pregnancy bleeding.
3. Determination of gestational age and fetal size assessment.
Fetal body measurements reflect the gestational age of the fetus. This is especially true in early pregnancy. In patients with late-stage menstrual periods uncertainty, such measurements must be made during pregnancy as early as possible in order to determine the correct age for the patient. See Frequently Asked Questions In the second trimester of pregnancy, measuring body parameters will allow the assessment of fetal size and growth and will greatly assist in the diagnosis and management of intrauterine growth retardation (IUGR).
The following measurements are usually made:
a) Rump length (CRL)
This measurement can be performed between 7 and 13 weeks, and gestational age can be very accurately estimated. The dating CRL can be within 3-4 days of the last menstrual period. (Table) It is important to note that when the due date is set by a precisely measured CRL, it should not be changed by subsequent scans. For example, if another scan after 6 or 8 weeks indicates that there should be a new, more distant deadline, the date should not normally be changed, but should be interpreted as explaining that infants did not grow as expected.
b) biparietal diameter (BPD)
The diameter between the two sides of the head. This is measured after 13 weeks. It increased from about 2.4 centimeters in 13 weeks to about 9.5 centimeters. Different infants of the same weight may have different head sizes, so dating late in pregnancy is often considered unreliable. (Charts and further comments) Appointments using BPD should be completed as soon as possible.
c) femur length (FL)
Measure the longest bones in the body and reflect the fetal longitudinal growth. Its usefulness is similar to BPD. It increased from about 1.5 centimeters in 14 weeks to about 7.8 centimeters. (Charts and Further Comments) Similar to BPD, dating using FL should be completed as soon as possible.
d) Abdominal circumference (AC)
The most important measurement in late pregnancy. It reflects more fetal size and weight, not age. Serial measurements can be used to monitor fetal growth. (Chart and further comment) AC measurements should not be used to date the fetus.
Here are other important measurements.
The use of polynomial equations that include BPD, FL, and AC can also very accurately estimate fetal body weight in any gestation. Computer software and search charts are readily available. For example, a 9.0 cm BPD and 30.0 cm AC will give a weight estimate of 2.85 kg. (Note)
4. Diagnosis of fetal malformations.
Many of the fetal structural abnormalities can be reliably diagnosed by ultrasound scanning, and these anomalies can usually be completed by 20 weeks. Common examples include hydrocephalus, anencephaly, myelodysplasia, achondroplasia and other dwarfism, spina bifida, exomphalos, Gastroschisis, duodenal atresia, and fetal hydrocephalus. With newer devices, conditions such as cleft lip / cleft palate and congenital heart abnormalities are easier to diagnose and at earlier gestational ages. (See also the FAQ and exception pages).
Early pregnancy ultrasound for the "abnormal" chromosomal markers, such as the lack of fetal nasal bone, increased fetal neck translucency (posterior neck region), is currently used to detect Down Syndrome fetus.
Ultrasound can also aid in other diagnostic procedures for prenatal diagnosis such as amniocentesis, chorionic villus sampling, umbilical cord aspiration (percutaneous cord blood sampling), and fetal therapy.
5. Placental localization.
Ultrasonography has become an indispensable factor in the positioning of the placenta and the determination of its lower edge so that the placenta previa can be diagnosed or eliminated. Other placental abnormalities such as diabetes, hydrocephalus, Rh alloimmunization, and severe fetal intrauterine growth retardation can also be assessed.
6. Multiple pregnancies.
In such cases, ultrasonography is invaluable in determining the number of fetuses, chorionic traits, evidence of fetal presentation, growth retardation and fetal abnormalities, the presence of placenta previa, and any suggestion of twin transfusions.
7. Hydramnios and oligohydramnios.
The amount of fluid (amniotic fluid) that is either too much or too little can be clearly delineated by ultrasound. Both of these conditions can have adverse effects on the fetus. In both cases, ultrasonography should be carefully examined to rule out fetal intrauterine growth retardation and congenital anomalies such as intestinal atresia, fetal edema or abnormal renal development. See also common questions and comments.
8. Other regions.
Ultrasonography is of great value to other obstetric diseases, such as:
a) Confirm intrauterine death.
b) Confirm fetal presentation in case of uncertainty.
c) Evaluate fetal movement, tone and respiration in biophysical profiles.
d) Diagnosis of uterine and pelvic abnormalities during pregnancy, such as fibroids and ovarian cysts.
Follow our facebook page to get newest information of our company and products.
Posted in News
By